Tongue Frenum Percing and Transdermal Implants: Difference between pages
(Page conversion via llm-mediawiki-rev -jwm) |
(Page conversion via llm-mediawiki-rev -jwm) |
||
| Line 1: | Line 1: | ||
[[File:TransdermalImplant.jpg|thumb|right|258px]] | |||
[[File:Small_spikes.jpg|thumb|right|260px]] | |||
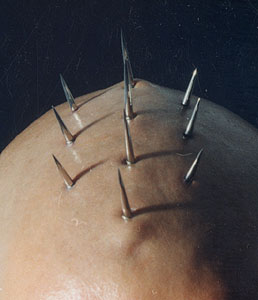
A '''transdermal''' (percutaneous) '''implant''' falls somewhere between a single-hole [[Pocketing|pocketing]] and an [[Category:Implants|implant]]. The simplest way to describe it is as a labret stud with the flat part under the skin, or "a piercing without an exit." The visual effect is that of jewelry (a bead, spike, etc.) that appears to be screwed right into the body. The invention of transdermal implants is credited primarily to [[Steve_Haworth|Steve Haworth]], and his design of the transdermal jewelry base made more effective [[Dermal_anchoring|dermal anchoring]] designs possible as well. The first transdermal implant was the "Metal Mohawk" that Steve implanted into Joe Aylward in [[1996]], [http://www.zentastic.com/blog/2012/07/26/the-transdermal-implants-of-samppa-von-cyborg/ [1]] and it lasted almost a decade before Joe requested to have it removed for personal reasons. | |||
The legality will, of course, vary from place to place, but it's hard to say exactly how courts would interpret transdermals. While the end effect is not that different from a piercing, the procedure itself is radically more complex. Whatever the legal interpretation of transdermals are, it is safe to assume that related issues such as the illegal use of anesthetics could pose problems for non-medical practitioners. | |||
== | It should also be noted that in most cases the visual effect of transdermal implants can be mimicked with [[Dermal_Anchoring|Dermal Anchoring]] and [[Surface_Piercing|Surface Piercing]]. | ||
* [[ | |||
* [[ | {{TOC}} | ||
* [[ | |||
==Jewelry== | |||
Successful healing requires proper jewelry that is more complex than simply using a labret stud, which will reject. Effective transdermal jewelry generally resembles a flattened pretzel, a figure eight, a clover, or even just a strip, with a short bar coming out at ninety degrees. The holes in the base are intended to help anchor the jewelry by allowing tissue to grow through them and closing up the pocket that was created during insertion. Making this specialized jewelry requires advanced machining facilities or titanium casting access. | |||
==Procedure== | |||
Performing the implant procedure requires advanced tools, techniques, and an experienced hand. The procedure itself involves making an incision approximately an inch from the desired implant location, creating a pocket under the skin for the jewelry to reside in, and exposing the bar through a hole created by cutting or dermal punch. | |||
In most cases, the procedure goes like this: | |||
1. The location where the transdermal passes through the skin is marked, as well as an incision point (usually an inch or two away). | |||
2. The incision is opened with a scalpel and a dermal elevator (often a septum elevator) is used to create a pocket to slide in the implant. | |||
3. Using a dermal punch or scalpel, and using the elevator as a backing (so underlying tissue isn't damaged), the hole that the implant will pass through is made. | |||
4. Through the first incision, the base of the transdermal is slid in, until its post passes through the hole. If the implant is two parts, the top half is screwed on. | |||
5. The initial incision is closed with sutures or suture tape. | |||
==Healing and Aftercare== | |||
It is very important to note that transdermal implants can be very difficult to heal. Many tend to stay in a continual state of "not fully healed" and often have scarred and irritated skin surrounding them. Healing can take up to two years to complete. Rejection can occur even after the transdermal is fully healed if it is accidentally bumped (though this is true of any surface piercing as well). However, while success is by no means guaranteed, there are several people who have managed to keep theirs for several years, even as long as a decade or more. | |||
==Related Risks== | |||
* [[Inward_Travelling_Infection|Inward Travelling Infection]] | |||
* [[Deep_Transdermal_Placement|Deep Transdermal Placement]] | |||
* [[Rejection|Rejection]] | |||
* [[Keloid|Keloids]] | |||
* [[Hypertrophic_Scarring|Hypertrophic Scarring]] | |||
* [[Bruising#Bruising_from_heavy_mods|Bruising]] (temporary usually) | |||
* [[Transdermal_Implant_Removal|Transdermal Implant Removal]] is becoming more common as time goes by, usually due to these risks. | |||
* [[Implant_Rejection|Implant Rejection]] | |||
==See Also== | |||
* [[Implant_FAQ|Implant FAQ]] | |||
Latest revision as of 21:14, 25 September 2023
A transdermal (percutaneous) implant falls somewhere between a single-hole pocketing and an. The simplest way to describe it is as a labret stud with the flat part under the skin, or "a piercing without an exit." The visual effect is that of jewelry (a bead, spike, etc.) that appears to be screwed right into the body. The invention of transdermal implants is credited primarily to Steve Haworth, and his design of the transdermal jewelry base made more effective dermal anchoring designs possible as well. The first transdermal implant was the "Metal Mohawk" that Steve implanted into Joe Aylward in 1996, [1] and it lasted almost a decade before Joe requested to have it removed for personal reasons.
The legality will, of course, vary from place to place, but it's hard to say exactly how courts would interpret transdermals. While the end effect is not that different from a piercing, the procedure itself is radically more complex. Whatever the legal interpretation of transdermals are, it is safe to assume that related issues such as the illegal use of anesthetics could pose problems for non-medical practitioners.
It should also be noted that in most cases the visual effect of transdermal implants can be mimicked with Dermal Anchoring and Surface Piercing.
Jewelry
Successful healing requires proper jewelry that is more complex than simply using a labret stud, which will reject. Effective transdermal jewelry generally resembles a flattened pretzel, a figure eight, a clover, or even just a strip, with a short bar coming out at ninety degrees. The holes in the base are intended to help anchor the jewelry by allowing tissue to grow through them and closing up the pocket that was created during insertion. Making this specialized jewelry requires advanced machining facilities or titanium casting access.
Procedure
Performing the implant procedure requires advanced tools, techniques, and an experienced hand. The procedure itself involves making an incision approximately an inch from the desired implant location, creating a pocket under the skin for the jewelry to reside in, and exposing the bar through a hole created by cutting or dermal punch.
In most cases, the procedure goes like this:
1. The location where the transdermal passes through the skin is marked, as well as an incision point (usually an inch or two away). 2. The incision is opened with a scalpel and a dermal elevator (often a septum elevator) is used to create a pocket to slide in the implant. 3. Using a dermal punch or scalpel, and using the elevator as a backing (so underlying tissue isn't damaged), the hole that the implant will pass through is made. 4. Through the first incision, the base of the transdermal is slid in, until its post passes through the hole. If the implant is two parts, the top half is screwed on. 5. The initial incision is closed with sutures or suture tape.
Healing and Aftercare
It is very important to note that transdermal implants can be very difficult to heal. Many tend to stay in a continual state of "not fully healed" and often have scarred and irritated skin surrounding them. Healing can take up to two years to complete. Rejection can occur even after the transdermal is fully healed if it is accidentally bumped (though this is true of any surface piercing as well). However, while success is by no means guaranteed, there are several people who have managed to keep theirs for several years, even as long as a decade or more.
Related Risks
- Inward Travelling Infection
- Deep Transdermal Placement
- Rejection
- Keloids
- Hypertrophic Scarring
- Bruising (temporary usually)
- Transdermal Implant Removal is becoming more common as time goes by, usually due to these risks.
- Implant Rejection